Spinal disease

The spine is the basis of the human musculoskeletal system. It consists of vertebrae, each of which connects with the neighboring ones at three points: the intervertebral disc in front, and two intervertebral joints from behind.
The mobility of the spine, its elasticity and elasticity, and the ability to withstand large-scale imaging loads are provided by intervertebral discs that are in close anatomical and functional connection with all spinal formations that form the spinal column.
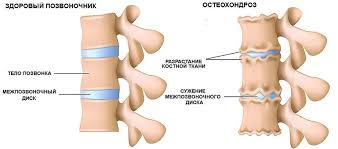
Osteochondrosis is a degenerative-dystrophic disease of the spine. Modern medical diagnosis - dorsopathy.
At the heart of the process is the change in the disc, its "drying out," a decrease in height, with the possible formation of herniated discs (penetration, bulging of the pulposal nucleus through the fracture of the fibrous ring of the disc). Thus, in the first place, the disk loses its functions of the active element - the properties of the shock absorber. With a significant swelling of the fragment of the disk, it is possible to squeeze the spine (radiculopathy), vessels (radiculohe- michemia), spinal cord (myelo-ischemia). This process is known under the traditional name "radiculitis". In this situation, pain can be not only local in nature, but also transmitted to different parts of the hands and feet, depending on the affected segment of the spine.
In connection with the loss of the disc of elasticity, the intervertebral joints in which osteoarthritis - spondyloarthrosis is formed, which also causes pain, are subjected to increased stress.
In response to the processes occurring there is a reflex protective muscular spasm, designed to fix the unstable affected segment of the spine. Despite the protective role, muscle spasm is another major cause of pain in osteochondrosis.

The following factors can influence the development of osteochondrosis:
· hereditary predisposition
· mechanical factors - injuries (sprains, fractures, dislocations) excessive strain on the spine
· hormonal disorders
· scoliosis, flat feet, spinal cord anomalies, a difference in the length of the limbs, and diseases of large joints.
General recommendations to the patient.
Despite the presence of signs of osteochondrosis on the radiograph, in the early stages they may not be accompanied by clinical manifestations.
With the development of the disease there are pains in various parts of the back, in the limbs, headaches. Pain is usually accompanied by a restriction of mobility. It should be remembered that similar signs are found in other diseases (pathology of the kidneys, female genital organs, gastrointestinal tract, various diseases of the nervous system, etc.). If back pain occurs, it is necessary to consult a doctor who, based on complaints, history the development of symptoms of the disease, radiographs and, if necessary, additional research methods, establish a diagnosis and prescribe the right treatment.
Avoid positions and movements that are unfavorable to the spine. To stand or walk follows with a straight back. Correct posture when the stomach is retracted and the thorax protrudes forward. If you have to stand for a long time, use a support, or from time to time move your body weight from one leg to the other. Avoid sudden movements. Wear comfortable and light clothing. Shoes should be on a low wide heel with a soft, elastic sole. Worsens the condition of the spine and intensifies the pain of fast and prolonged walking, especially on uneven roads.
If you sit, then try not to strain your neck and shoulders, rest your feet on the floor. To maintain a straight back, place a small pillow behind the waist. when driving a car it is advisable to use a special orthopedic pillow under your back. Choose an armchair or chair with a high back supporting the spine.
If you lie the spine should always be straight. First of all, you should pay special attention to the sleeping place. The bed should be chosen elastic, but rather rigid, giving preference to orthopedic mattresses and pillows. Put a small pillow under your neck, and in case of pain in the lumbar region - and under your knees.
If you lift and carry weights, always check the weight of the object and if it is too heavy - do not lift it. When moving the load, use the power of the hands or feet, not the back. Items lift in two stages. First, while sitting on your knees, placing a roller under them, keep the object closer to the body. Then gradually rise. Try to always evenly distribute the weight of the weights carried by using both hands.
Methods of treatment of osteochondrosis
Orthopedic correction
It is important for osteochondrosis to correct flatfoot using foot restorers and orthopedic shoes. In some cases, doctors recommend using special corsets. You need to know certain restrictions: a corset can be worn for no more than two hours straight and no more than six hours a day. Violation of the recommendations can lead to further weakening of the back muscles and worsening of the course of the disease.
Physiotherapy
· It is not recommended to perform exercises from books, magazines, seen on TV, from the words of other people. Executing an incorrectly interpreted exercise can cause serious harm.
· It is necessary to select an individual set of exercises for the physician of physiotherapy exercises.
· Exercises should be aimed at strengthening the muscles of the back, and do not carry an additional burden on the spine.
· Exercises should be performed regularly with a gradual increase in volume and load.
· Vigorous movements through acute pain are not desirable.
Manual therapy, acupuncture, physiotherapy
These methods are widely used and have an effect aimed at relaxing the muscles, reducing pain and improving mobility of the spine and joints. However, it should be remembered that these methods have serious limitations and in some cases their illiterate use can lead to deterioration.
The symptomatic medication is prescribed by the doctor depending on the severity of these or other symptoms.
Minimally invasive procedures for surgical treatment for prolapses and protrusions of discs
· Chymonucleolysis
· Plasma low-temperature evaporation of a disk
· Risotomy
· Microdiscectomy
Prophylaxis of pain in the back
The concept of preventing spinal column disorders is not widely used, and this sad situation remains true not only with regard to back pain, but also health in general. In fact, everything is quite simple. Healthy people do not have enough motivation to actively engage in prevention. They wait for the back to get sick (or another disease will appear), and then try to correct the situation and prevent repetition. If you already had an attack of pain, therefore, it is possible that within a year it will recur. Practice shows that this happens in 50% of those suffering from back pain. The second attack is usually weaker than the first one. The second attack happens because people forget the lesson of the first. They return to their habits, pick up heavy objects, become too tense and sit too long in one place. Do not make yourself worse. Remember, because of what was the first attack. Do exercises, rest, when required, and do things at certain times of the day. If you follow these simple tips, the second attack is unlikely. Here are my tips on how to avoid back problems or prevent them from repeating. Do not smoke Try to quit smoking - it will be better for the back, lungs, heart and other organs. All the tissues of your body require oxygen for work, and smoking steals it, especially in the spinal discs.
If the blood contains less oxygen, then the disks respectively receive it less, and this can cause the process of their fragmentation, which increases the risk of a hernia. Maintenance of the form If you are in good physical shape, the risk of lumbar pain is unlikely. We can give you some tips on how to maintain a good state. For example, a good condition of the cardiovascular system is the ability to go down and climb the steps without difficulty breathing. It is noticed that firefighters in good physical form have a lower risk of back pain than those with weak physical development. Strong back muscles are another sign of good shape. Muscles of the back are mostly weaker than other muscles of the body, which means that if we increase their strength, we will reduce the risk of back pain. This is important for everyone and especially for those who lift weights, do heavy physical work. Exercises that strengthen the abdominal and back muscles reduce the risk of pain if you lift heavy objects and flex and straighten out during work. To maintain a good shape of the whole body, do a total exercise every day. In the weekend, you can remove muscle fatigue. Be engaged in strong, vigorous exercises within 30 minutes to stimulate a diaphoresis. The appearance of sweat means that you used enough calories to cause sweating, which is responsible for the sympathetic nervous system - part of the nervous system that prevents pain. These exercises also improve blood circulation, flexibility and muscle tone. Maintaining normal weight Completeness is not a risk factor for back pain, but it prevents proper exercise. If obesity is the result of a sedentary lifestyle, then the risk of developing any diseases is quite high. The body mass index (BMI) of a person is either satisfactory or not. For example, if your height is 6 feet and your weight is 200 pounds, then the BMI is 27, which is a lot for you, you need to weigh 170 or 180 pounds. With an increase of 5 feet and a weight of 150 pounds, the BMI is 25. Data from the national health institutes diagnose a threat of obesity if the BMI exceeds 25.
Obesity begins if it is 30. Getting a lot of antioxidants Make sure that your diet contains a large amount of fruits and vegetables that are sources of vitamins A, C, E (antioxidants). Beta-carotene is found in green and yellow fruits and vegetables, such as cantaloupe, apricots, spinach and carrots. Dairy products and eggs contain vitamin A, citrus - vitamin C, vegetable oils - vitamin E. There is as yet no exact scientific data on the direct effect of antioxidants on intervertebral discs. Despite this, I believe that antioxidants are related to the reduction of oxidative back pain and that the functions of the discs are improved by this therapy. The appropriate dose of antioxidants, mainly from food, is important for maintaining the health of the spine. Free radicals are involved in the aging process, including the spine. At autopsy in people from 13 to 86 years old, oxidative damage was found in the cartilaginous cells in the center of the discs. And in all cases, attempts were made to "repair" the oxidative damage. All this proves that the degeneration of disks due to the oxidative process begins in the second decade of life. Active oxygen molecules (free radicals) damage the cells of the back disks. Cells try to act on molecules, but this action is ineffective, and the disks only wear out faster. Antioxidants (vitamins E, A, C and beta-carotene) can neutralize the destructive effect of oxygen radicals. If you take these substances as supplements, keep in mind that vitamins A and E are rather slowly absorbed by fat and removed from the body. Their excess can be harmful. Increased risk of kidney stones and the development of diarrhea; when too much vitamin C is taken, bleeding increases in people taking anticoagulant medications, and excess vitamin E leads to brittleness of hair and nails due to accumulation in the body of selenium. The dose of vitamin A equal to 100,000 units is toxic. The National Academy of Sciences recently set the intake limit vitamins C and E, as well as mineral selenium:
· vitamin C - 2000 mg;
· vitamin E (synthetic) - 1100 mg;
· selenium - 400 mcg.





